Diversion colitis is also known as diversion proctitis. Diversion colitis usually occurs after an individual has experienced ileostomy or colostomy surgery and part of the large intestines have been salvaged. Diversion colitis is when the large intestine has inflammation and if the rectum is inflamed, it is referred to as diversion proctitis. Diversion colitis also occurs in individuals who suffer from inflammatory bowel syndrome. Diversion colitis occurs more frequently with individuals who have inflammatory bowel syndrome than with individuals who have had colostomy or ileostomy surgery. When people experience diversion colitis, there may be symptoms, but in most cases, there are no symptoms present.
The Causes And Risk Factors Of Diversion Colitis
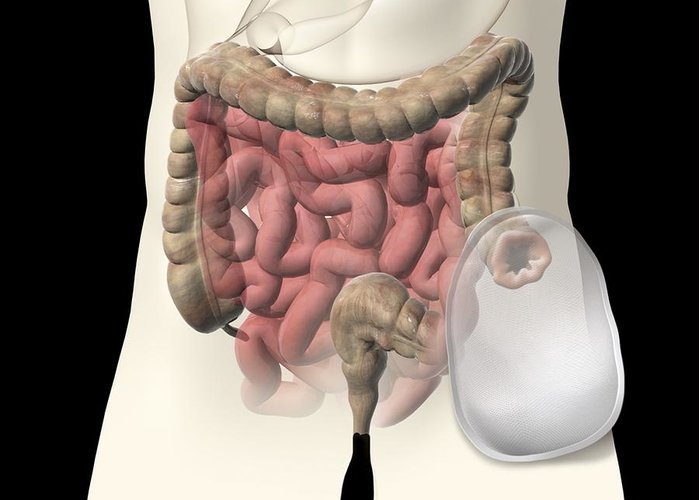
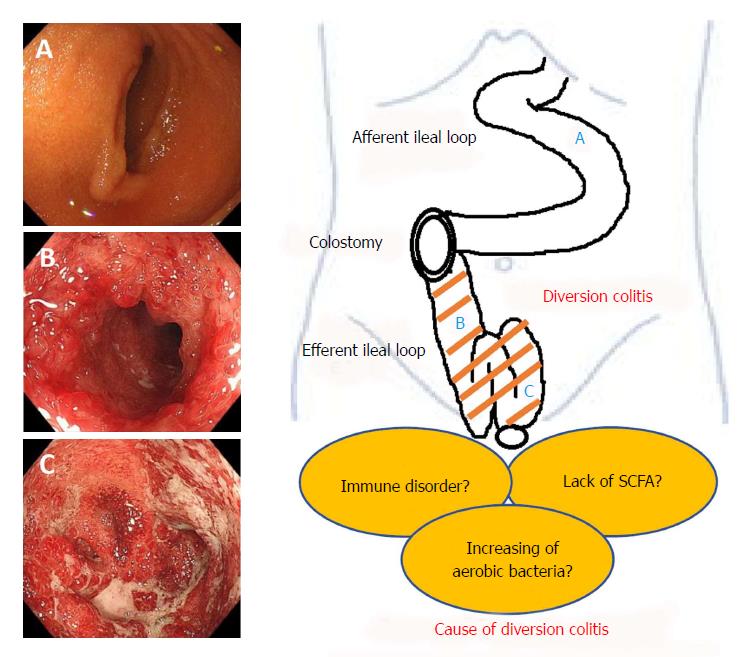
No one in the medical community, including doctors, can explain precisely why diversion colitis occurs. Doctors know that it happens when part of the large intestine is left in place due to an ostomy. Doctors have come up with a theory about diversion colitis and its cause. They state that it occurs because a part of the large intestine is left in place, but it is not being used to create and process stool. So basically, the lack of usage of the large intestine that is left in place after an ileostomy or colostomy is put in place is the most likely reason why diversion colitis occurs.
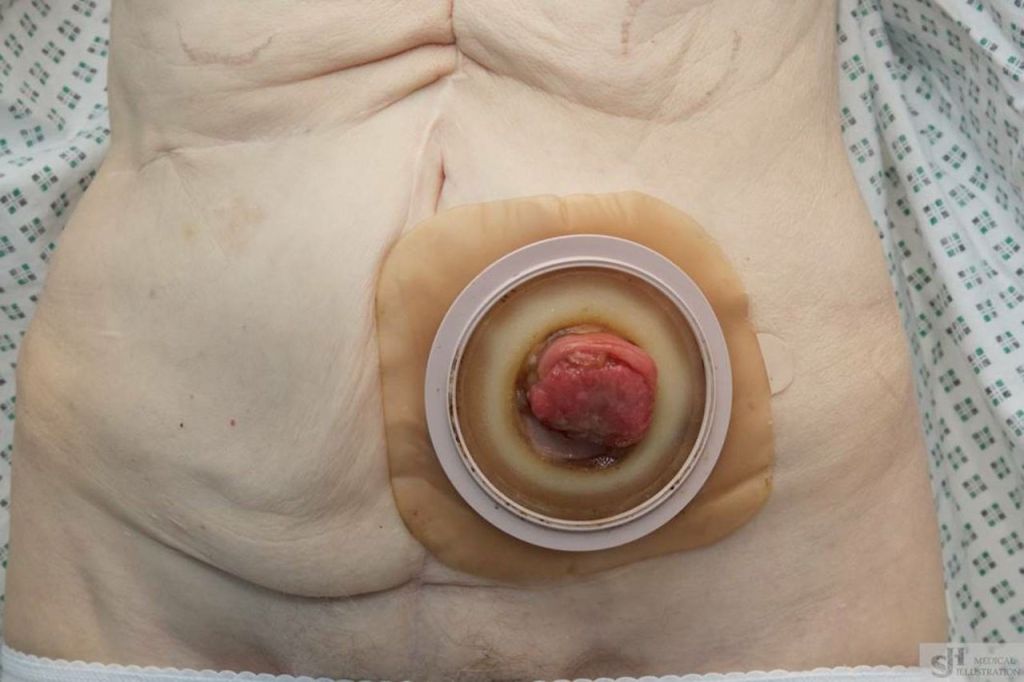
Most people at risk of developing diversion colitis are again, as stated previously in the article, who have had ostomy surgery. People who also experience irritable bowel syndrome, have diverticular disease and have had colorectal cancer can also develop diversion colitis. People who suffer from irritable bowel syndrome develop the disease the most out of all the people at risk of developing the disease. When it comes to individuals who have ostomy surgeries, the research is not pinpoint accurate on the amount at risk of developing diversion colitis. The studies that have been done show that between 70 to 100% of patients will develop diversion colitis. Looking at these percentages, it is clear that this is a very broad range and this is why it is difficult for doctors to determine how many ostomy patients are genuinely at risk.
The Symptoms And Treatment Of Diversion Colitis
In many cases, a patient who experiences diversion colitis has no signs and symptoms. The main reason why is that inflammation of the colon is not something that an individual can feel. If symptoms of diversion colitis occur,—it is usually abdominal pain, rectal bleeding, an urgent need to empty the bowels, and rectal discharge. There are two ways that diversion colitis can be detected or diagnosed. The first way is through a white blood cell count test and the second way is by endoscopy.

The best treatment for diversion colitis is for the ostomy to be reversed and this procedure is known as a take down. A take-down procedure is when the ostomy is reversed and the large intestine is reconnected and begins to function as expected. A take down is done when whatever underline disease such as cancer or ulcerative colitis has been effectively treated. Short-chain fatty acid enemas are an excellent way to treat diversion colitis. These enemas have to be administered or taken by the individual twice a day. Another enema that can be taken twice daily and is effective in treating diversion colitis is glutamine enemas and they are also called butyrate enemas.